Antithrombotics
Antithrombotics in Endoscopy:
Consider:
- Bleeding related solely to antithrombotic
- Bleeding related to an endoscopic intervention performed in the setting of antithrombotic use
- Thromboembolic event related to interruption of antithrombotic therapy
Low risk of bleeding during procedure:
- All diagnostic procedures including mucosal biopsy
- ERCP without sphincterotomy
- Diagnostic DBE
- EUS without FNA
- CE
- Stent deployment without dilatation
High risk of bleeding during procedure:
- Polypectomy
- Therapeutic DBE
- ERCP with sphincterotomy
- Procedures with bleeding potential in an unaccessible site or uncontrollable with endoscopic means
- PEG
- EUS with FNA
- Dilatation
- Endoscopic haemostasis
- Tumour ablation
- Variceal treatment
Low risk of thromboembolic event:
- DVT
- AF without valvular disease
- Bioprosthetic valve
- Mechanical valve in aortic position
High risk of thromboembolic event:
- AF with valvular disease
- Mechanical valve in mitral position
- Mechanical valve with a previous thromboembolic event
- DES on DAT < 1 year, BMS on DAT < 1 month
- EF <35%
- H/O thromboembolic event
- Age >75 y.o.
- ACS
- Non stented PCI after MI
Rate of major embolism in patients with mechanical valves
- In absence of antithrombotic therapy is 4 per 100 patient years
- With antiplatelet 2.2 per 100 patient year
- With warfarin 1 per 100 patient year
AF which is nonanticoagulated has an annual stroke rate of 4.5%
ELECTIVE ENDOSCOPY:
Risk of continuing antiplatelets:
Diagnostic endoscopy:
No bleeding in endoscopy with or without biopsy while taking either ASA of clopidogrel
Even warfarin is safe for low risk endoscopy with or without mucosal biopsy in OGDS and Colonoscopy
Colonoscopic polypectomy:
ASA/NSAID has low post polypectomy bleeding
Warfarin within 1 week has a higher risk of bleeding which polypectomy clip doesn’t prevent.
Sphincterotomy (0.3 – 2%) and PEG (2.5% bleeding without antithrombotics):
Anticoagulation within 3 days increases risk of bleeding
ASA / NSAID for 7 days hasn’t been shown to reduce the risk of bleeding
Risk of stopping antiplatelets:
Absolute risk of an embolic event whom anticoagulation is stopped 4 – 7 days is 1%
If antithrombotics are temporary and the procedure can be delayed, it should be delayed till after stopping antithrombotics
Reinitiation of antithrombotics:
No consensus on the optimal timing of restarting antithrombotics
If low risk, attempt to restart within 24 hours while if high risk, to restart as soon as bleeding stability allows
ACUTELY BLEEDING PATIENTS
No prospective data to determine safe level of INR for endoscopic therapy.
INR < 2.5 seems to be safe
Restarting antiplatelets within 1 week increases bleeding by 2x (19% vs 11%) but the risk of mortality at 2 months improves markedly (1.7% vs 14.5%)
Others:
Minimum DAT for BMS is 1 month and DES is 1 year
ASA alone has more safety data than Clopidogrel alone once DAT period over.
GIB in ACS: 4 – 7 fold mortality than ACS alone
Endoscopy risk is up to 12% on same day of ACS, usually 1 %
GIB leading to ACS has a higher risk of needing endoscopic treatment compared with ACS followed by GIB
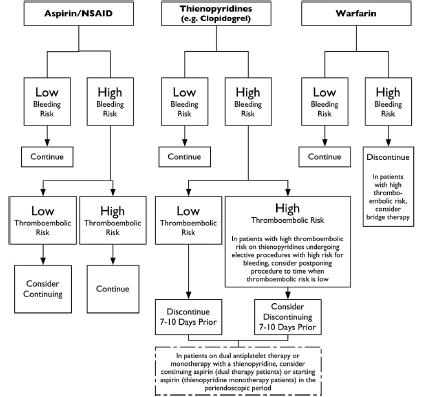
Antithrombotics in elective setting
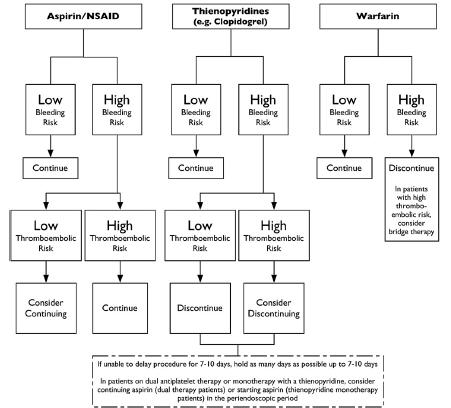
Antithrombotics in emergency setting
edited 16th July 2010